We use cookies to help provide you with the best possible online experience.
By using this site, you agree that we may store and access cookies on your device. Cookie policy.
Cookie settings.
Functional Cookies
Functional Cookies are enabled by default at all times so that we can save your preferences for cookie settings and ensure site works and delivers best experience.
3rd Party Cookies
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Mental Illness and Suicide
When do we say enough is enough?
Practitioner Health - Increasing numbers and increasing severity
Over the last 12 months NHS Practitioner Health has registered around 6,000 new patients presenting for care. Most are doctors, with more than forty per cent being GPs.
At registration, patients are asked to complete validated questionaries looking at anxiety, depression, stress, and wellbeing. This includes questions asking about suicidal thoughts or plans to end life.
Almost all patients reach the threshold for a formal diagnosis of mental illness, most commonly moderate to high levels of anxiety and depression.
When using the free text function patients are recorded feeling overwhelmed and struggling with their workload, this trend increasing even since the height of the pandemic.
In September 2022 work pressures overtook anxiety for the first time since the start of the pandemic.
It has become increasingly common for patients to record feelings of guilt, unfairness, and anger around what they have experienced in the last few years. These emotions form the cluster of what we now understand to be ‘moral injury’.
Others report a cluster of symptoms that might be identified as burnout, including fatigue, emotional exhaustion, and loss of compassion.
Suicidality
Around one third of the patients presenting to Practitioner Health have reported that they have thought about ending their own life or have made actual plans to kill themselves before seeking help. Many report that workload and demands of the job have become overwhelming and unmanageable and are the main reasons for their suicidal thoughts.
This figure has been rising in recent months from around 28% in October 2021 almost 36% in October 2022 – an increase of 8% from this time last year.
1836 people who registered with Practitioner Health in the last 12 months reported that they have had suicidal thoughts on several days, more than half of the days or nearly every day over the last 2 weeks prior to self-presentation.
Of those 1836 people, just under a third (496 people) had made plans to end their lives in the last week.
Practitioner health logs deaths of a health professional where suicide is deemed the cause. In the last 12 months, we are aware of 18 such deaths. This is likely to be an underestimate.
Survey carried out in October 2022
To try and understand whether GP patients attending Practitioner Heath were exceptional (that is by seeking help they were unwell and as such not representative of the general GP workforce) we undertook a survey during October 2022. This was carried out using social media.
We have had almost 300 responses during the month.
Questions asked:
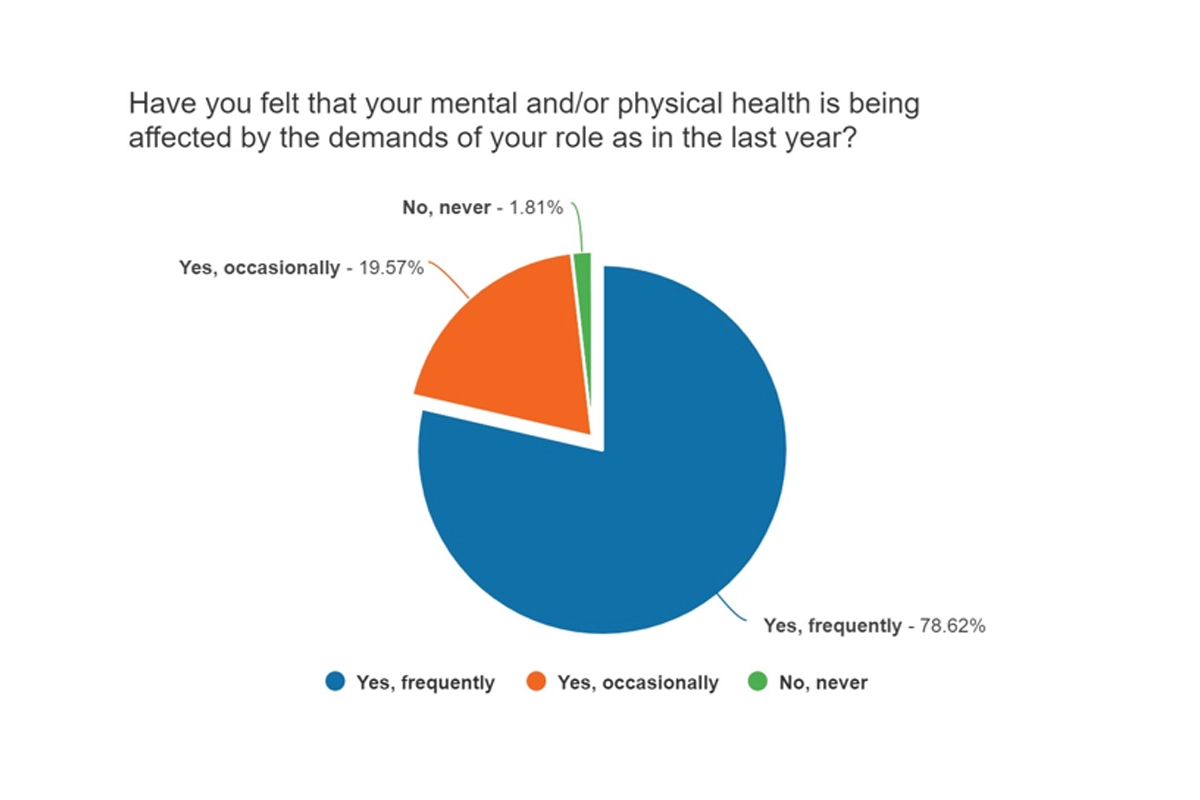
Have you felt that your mental and/or physical health is being affected by the demands of your role as in the last year?
Pie Graph depicting the following:
- 78.62% said "Yes, Frequently"
- 19.57% said "Yes, occasionally"
- 1.81% said "No, never"
98.19% of those completing the survey felt their mental or physical health had been affected by the demands of the job in the last year.
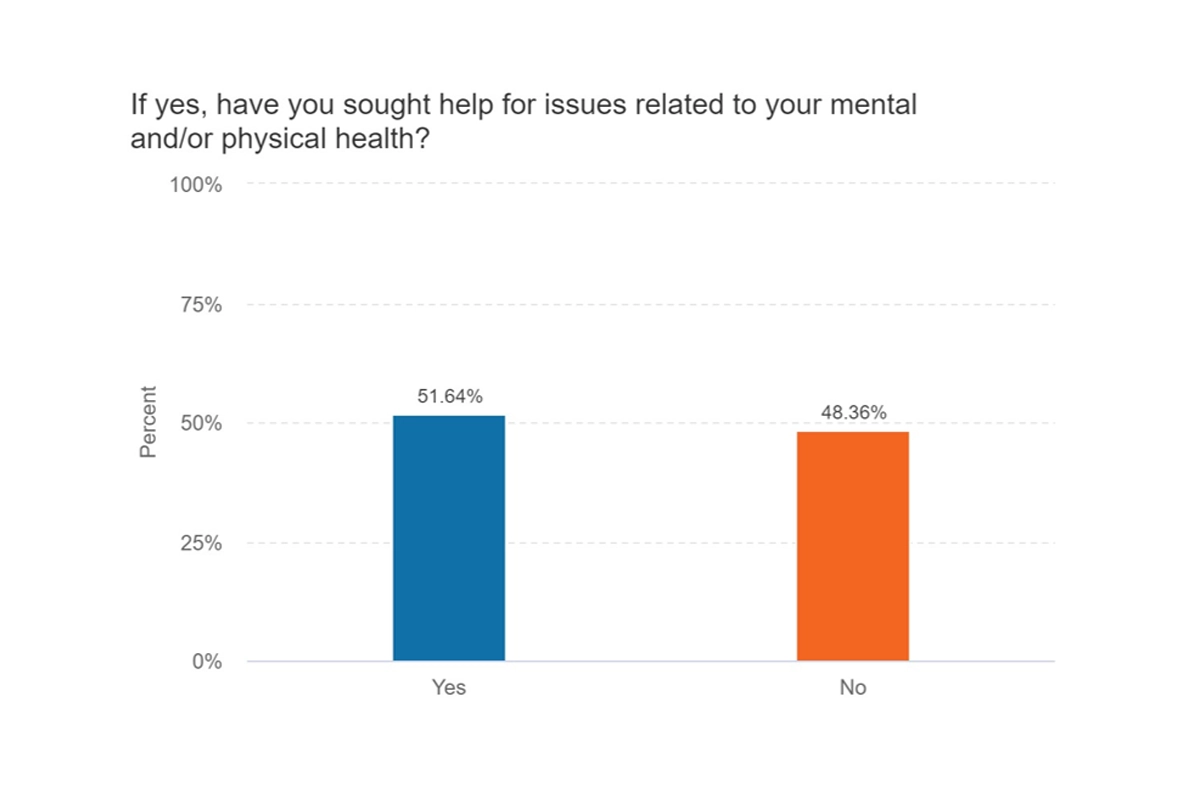
If yes, have you sought help for issues related to your mental and/or physical health?
Bar Graph depicting the following:
- 51.64% said "Yes"
- 48.36% said "No"
Almost half of those whose health had been affected by the demands of the job had not sought help.
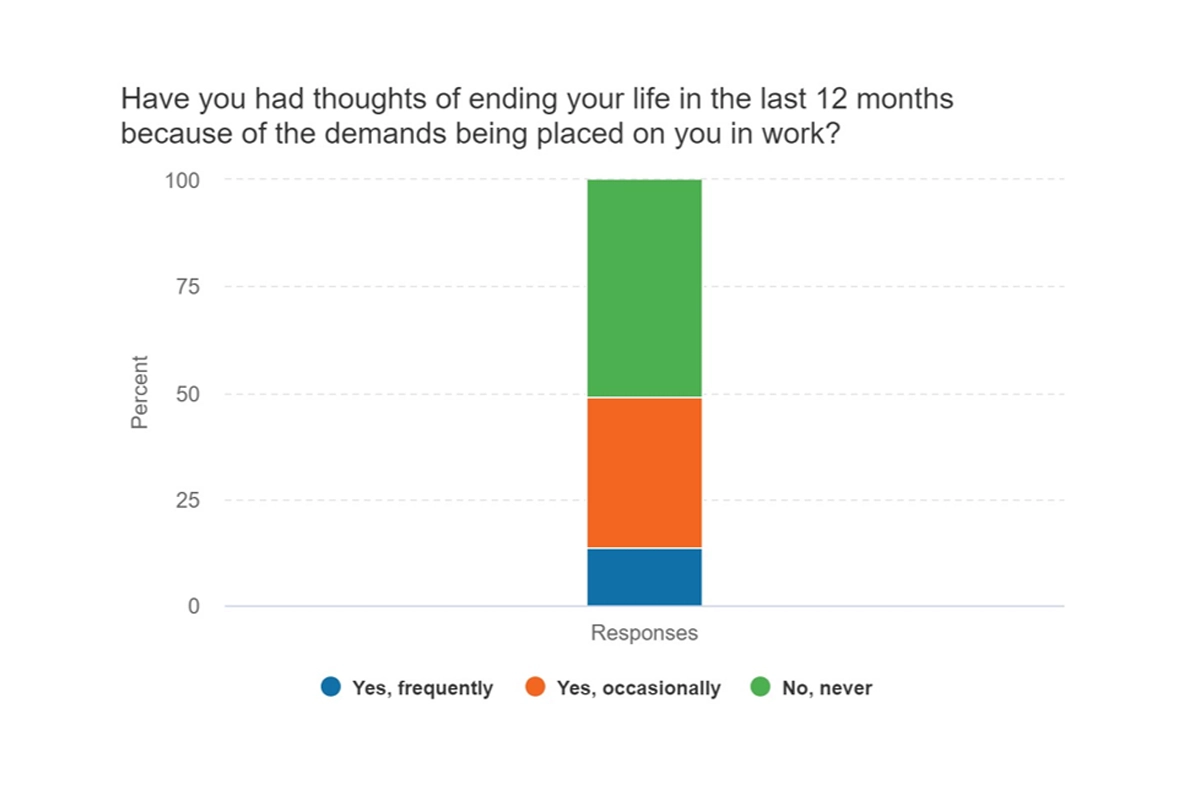
Have you had thoughts of ending your life in the last 12 months because of the demands being placed on you in work?
Pie Graph depicting the following:
- 13.5% said "Yes, Frequently"
- 35.4% said "Yes, occasionally"
- 51.1% said "No, never"
Almost half of those who completed the survey had thoughts of ending their life in the last 12 months, either occasionally (35.4%) or frequently (13.50%).
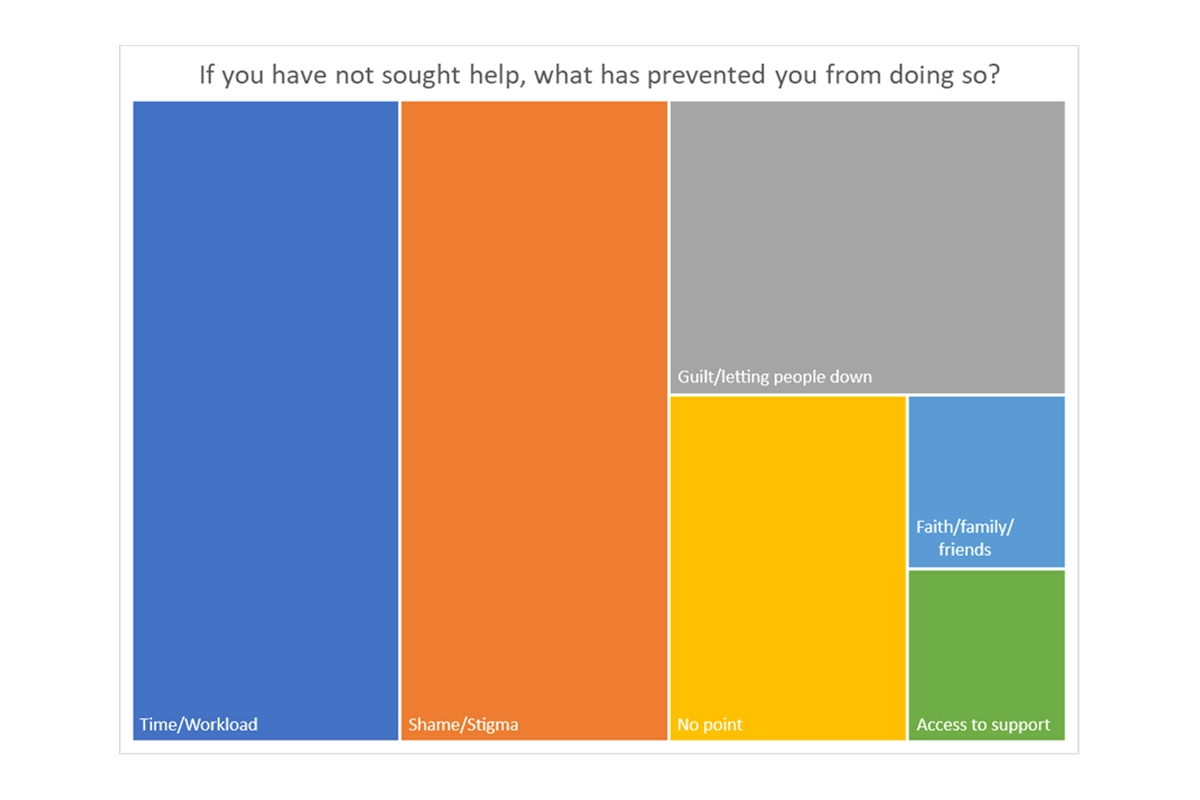
If you have not sought help, what has prevented you from doing so?
Graph depicting the following:
- Almost 30% of those who had not sought help had not done so due to pressures of workload or time.
- Around 28% had not done so due to shame or stigma whilst almost 20% had felt guilty that they would be letting people down if they did so.
- Around 14% felt there was no point in seeking help, nothing would change and described feeling helpless and around 4% felt they were not able to access the support they needed.
- A small proportion (around 4%) felt they had support from family/friends or their faith.
"It was difficult to seek help as did not recognise where I was, too busy trying to help others. Everyone is struggling so puts more pressure on colleagues/friends. Fortunately, my work colleagues had my back and supported me. I found myself in awe of the Dr that ended their life, “it is one way to stop everything,” including the ungrateful complaints from patients, families and many who do not recognise how much we all give."
"Eventually got some time off and the break that I needed but many, many months after I should have. Pressure to stay at work was immense. My decision making for myself became flawed. I put everything into being a good doctor for my patients. I resisted taking time out for so long."
Challenges
What needs to happen?
- Recognition of impact and toll of the last 2 to 3 years on mental health of workforce
- Recognition that staff numbers have gone down whilst patient demand has gone up
- Identification of limits for number of patient contacts or hours worked per session/day before patient safety becomes a factor
- Agreement of a safe ratio between clinical time and time to think/plan/reflect/learn
- National enquiry around suicide in H&C professionals
- A shift in thinking to reduce expectations on primary care - shift in what can be done in secondary care eg allowing referrals between secondary care clinicians rather than back to GP or direct access for patients to some areas in secondary care
If not, why not?
- I am trying to the job of 2 people the workload is never ending . It’s not safe I feel mistakes are going to me made.
- The current situation overall is unsustainable It feels as if we are the mule in Buckaroo, deliberately being overloaded with the sole purpose of making us snap under the strain.
- Hospital doctors need to stop dumping work on GPs e.g. arrange their own follow up appointments, do their own investigations ( and give the patient these results), do their own referrals.
- Ill- conceived recommendations which increase GP workload need to stop e.g. ‘see your GP before exercising’ or ‘all women to be offered a menopause health check aged 45’.
- There is no cap on what comes into GP. No limit. It is impossible to do a good job.
- Need to be honest with public that other health professionals will see them rather than a GP e.g. First contact physiotherapists, PAs, pharmacists
Individual Comments
- Constantly tired, irritable, snappy at home, resentful, no time for any enjoyment. I have frequently wondered if I am depressed but then I have a week off work and feel better. I've done online learning about burnout and the impact on physical and mental health. But there just isn't time to acknowledge that you're struggling as everyone else is. Spend time supporting colleague who are equally struggling.
- The workload is increasing, combined with an already exhausted workforce who are battered by the public and press. There feels like there is no let off and it won't take much more to break the system and the individuals working within it.
- Insomnia, palpitations, anxiety…for the first time in my 25 years plus as a doctor, work has overwhelmed me. The public and press criticism has made me question my future. It’s like running on a treadmill where you can’t get off unless you fall. The demands are never ending and the expectations unable to be met. I feel so sorry that the NHS is failing people, and GPs are trying their very best but the workforce is not there to offer the service we all want. In my practice several doctors have resigned or taken early retirement as the pressure was too much, those left behind are struggling every day. My physical health is affected, my family relationships have deteriorated, and my mood is at an all time low. I have always seen myself as strong resilient and capable until this year, now I just count the days until I too can walk away. I though I’d work until we’ll into my 60s but with the pressures I'm now thinking 55 is more likely. The NHS is doomed unless we can turn things around and that will take a change in tack of the government, patients, and the press. We need the autonomy that allows doctors to treat those “who need” rather than those “who want”, the complaint culture has meant we bend over too far for those who demand, rather than given care to those who truly need. General practice has become a sticking plaster to deal with all the social issues in our country and it is now crumbling quickly. ….sorry you asked!!
- I could be really good at my job if I had time and space to think. Instead, I am stressed, overwhelmed and terrified of making a mistake. I am trapped being a GP by being the main earner in my family but wish I could walk away. 10 years ago, I loved my job and now I hate it.
- The system itself feels like a sinking ship with no lifeboats. It’s difficult to talk about this with others at work because you know they are struggling too. We are all trying to be there for each other and normally there are enough people doing okay, keeping the ship afloat and with the strength to pull you back aboard, but when you are all drowning you all just pull each other under and sink.
- The constant media bashing is soul destroying. We need a media campaign to explain what the primary care team is and does. It’s not just the GP but NHS websites say “ask your GP.” We are swamped but we are a team and so the message needs to get out about how people can best use their primary care team, and when self help or pharmacy help etc would be suitable.
- With the workload being as it is. The only options seem to be to allow it to affect your mental health or leave I think there needs to be some recognition from NHS England on the impact of their decisions and the wider impact of poor mental health on the service delivery throughout the NHS. The more practitioners that leave the worse the burden is for those that are just about holding it together. Most other health practitioners such as counsellors have in built mentoring time into their timetable and although practitioner health is fabulous it's dealing with the problem after the horse has bolted.
- There is not a bottomless pit of reserve tank energy in the existing workforce, but demands still creep up and add on . I have had a successful return to work after severe episode of burnout/depression when I did feel suicidal and wasn’t sure if I should ever or could ever continue working as a doctor. I am back full time but having to be very strict about what I can or cannot offer in order to stay well and in work
- The high workload- extended hours, coming home late every day, feeling you give everything for your patient’s had severe negative impact on home life/relationships. Everyone is in same boat and heading for collapse. I often heard colleagues state they want to walk away but it is the people we work with that holds us. Pressures coming from all sides Buck stops with GP practice Drs Nurses, AHPs, reception, management and admin through to cleaning and waste management, we are all feeling it!
- Feel impossible to do anything right at the moment in NHS have had fleeting thoughts of would be easier if not Alive but not real concrete thoughts Feels impossible to be a GP at the moment I always feel not good enough or I'm not helping my patients enough and I cannot keep up with the admin I have a constant feeling I'm going to miss something and be sued
- People have no idea how we work, what we deal with on a day to day basis. Many people think ‘ I only need 5 mins of the Drs time’- they genuinely think it will take this time. No appreciation of the time, risk, thought processes, documentation involved in any consultation for even what may appear the most simple request. The vastness, complexity and lack of joined up clinical notes(GP & hospital) is alien to patients.
- I am beyond burnout. If I'm honest I've probably been through three or four "nervous breakdowns" in the past 30 years as a doctor, but managed to pull through by being utterly bloody minded. This match head is complete carbon and I'm numb. I will quit medicine as soon as I can.
- Being sandwiched between the government seemingly scapegoating GPs and accusing us of constantly failing, and patients who believe we are work shy with big shiny salaries makes you feel worthless as a human being. The role I believed I would have when I applied for medical school 15 years ago has disappeared. If we had support from either the government or our patients/general public, life may be more enjoyable. Instead it’s just working to survive and not enjoying that work but there are no careers out there to swap to where my skills would be of any use. So we are stuck in a constant pattern of depression/anxiety then burnout, time off, returning to work to make ends meet and so on. I honestly wish I hadn’t become a doctor as I believe my mental health wouldn’t have been so damaged by any other job.
- Constant pressure, can never do enough. Huge sadness that patients needs are not being met: patients with very reasonable requests and knowing that referral will take ages and the only support available in the meantime is me. Feeling like I can’t provide good quality care for my patients. Feeling unappreciated by the public - constant negative media
- It’s just too much and no end in sight, no recognition and understanding that we are giving everything to the job, doing our absolute best and there is nothing coming from government or the centre to suggest how and when things will change. People can only go on so long without hope or optimism that the situation will improve, that’s why those that can are leaving and others are exploring options. It’s devastating, we all want to do our best but it’s like we are fighting a losing battle every day
- Burnt out. Exhausted. Unable to be my usual self in the last 6-10 months due to Patients unrealistic expectations and media fuelling negativity. I get daily verbal abuse from patients. I’m too tired when I get home at 8-9pm to have an Honest conversation with husband. Physical and emotional Relationship affected. Respect is lost from the profession. Sadly. Will probs leave the NHS in next year or two To work in Australia
- I desperately want to leave my job/healthcare, but I don’t have the mental strength/capacity to apply for other jobs. I’m so sad at the thought of leaving a stable career I used to be proud of, but I know it’s necessary. I’ve suffered from horrific anxiety, panic attacks and depression due to work in the past and I don’t want to require medication just to get me through the working day.
- Working in a broken and under-resources NHS system is exhausting - because everyone is so tired, so stressed and hence unable to be the best version of themselves. Aside from the adverse impact that has on patient care/patient safety, overall productivity and creativity… it has just become a fundamentally negative working environment that most people cannot wait to escape.
- I burnt out and left my partnership due to demands of my role, especially during summer months where I was expected to cover others on Annual leave despite already working 3 days and reducing my hours to cope with the workload pressures. I was working 5 days a week in the end, logging on from home to start to prepare for next day so working through my days off. My breaking point was being the only doctor for over 10,000 patients, on call for the whole day only supported by a paramedic who I was also supervising, and expected to cover most of the admin in addition. I'm a broken mess my partners and the practice continues relentlessly. Also you need support of colleagues and a good team, if you're isolated or in a toxic environment protect yourself and get out. I do feel guilty still now when I see how primary care is struggling, I can only do what I can and I do fear for patient care and staff health and morale in the future.
- It seems like NHS GPs are just punching bags, no one cares & even our best is never enough, need an escape route but there doesn’t seem to be any way forward

